Coronavirus Disease 2019 (COVID-19)
COVID-19 Patient Care at Olive View
Important Pager/Phone Numbers
24-hour COVID ID Attending: pager 818-313-0057
2F Isolation Unit: x74440
Infection Control: x73624 or x74739
Administrative Nursing Office (ANO): x73170
Bed Control: x73179
Respiratory Therapy: supervisor x75038, lead x73331
** If dialing from a non work phone, you need to dial 747-210-**** (4 digit extension)
COVID Protocols & Workflows
Criteria for testing in AMBULATORY setting:
Use these instructions for obtaining Outpatient COVID testing (updated 2/2021)
Outpatient COVID Testing Instructions
If patient meets the above criteria and needs a clinical evaluation, please direct them to the Respiratory Urgent Care (Resp-UC) for testing. Please call Resp-UC to notify them about the patient (warm hand-off) and document a note.
If the patient does not need clinical evaluation, the patient may qualify for next-day drive-thru testing (drive or walk through) at Olive View. Same-day testing is not available.
- If the case is identified on Monday through Thursday:
- Ask the CMA to book for next-day COVID Drive Thru testing
- Provider needs to place the order for COVID test
- If it is a Thursday:
- The CMA will have to get approval for Friday testing (due to limited testing capacity on Fridays)
Criteria for testing in the INPATIENT setting:
Universal testing for admitted patients: All patients requiring hospitalization will be tested for COVID-19. Test results should be known prior to deciding the inpatient unit.
For suspected false negative test results, i.e. high suspicion of COVID-19 despite negative test, place a Request for Admit order with special instructions stating “High-risk PUI.” Continue enhanced precautions. The patient will be placed in isolation until further testing can be performed.
How to order the SARS-2 COV test?
Two order sets are available through ORCHID:
“Coronavirus COVID-19 (SARS-CoV-2) Testing” – use in Acute care settings (ED, inpatient, urgent care)
“AMB Coronavirus COVID-19 (SARS-CoV-2)” – use in outpatient clinic setting
In order to test for COVID-19 from the ED or Medicine Wards, please do the following:
- Use the COVID-19 order set and indicate the reason for the COVID-19 test order in the “COVID Test Approved by” yellow text box
-
-
- highest priority: critically ill patients, stable admit, PUI pending psych admit, asymptomatic admit, outpatient who cannot self-isolate
- standard priority: outpatient HCW, outpatient who can self-isolate, outpatient with high-risk medical conditions, USNS Mercy screening
-
You do not need to page the ID attending for pre-approved indications – all categories stated above are pre-approved. If you are unsure if your patient falls into these categories, please contact the COVID ID attending.
If re-testing is required due to false-negative test result, page the COVID ID attending in order to discuss indication fo retesting and setup alternative testing (different specimen site, different testing facility).
The lab will stratify the test:
-
-
- Highest priority patients will receive the fastest available testing first-come, first-served (outside of OV with <2 hour TAT for first 20 tests/day, then send out to an outside lab for an appx 24 hour TAT)
- Standard turnaround time will go to Quest Diagnostics routine for 24-48 hr TAT
-
Performing a Nasopharyngeal Swab: Nasopharyngeal Swab Technique (NEJM)
Reporting positive COVID-19 tests:
At this time, infection control (x73642) is reporting all positive tests to the Department of Public health.
Click here for guidance on telephone disclosure of a negative COVID-19 test result to a patient
Click here for guidance on telephone disclosure of a positive COVID-19 test result to a patient
Guidance on Inpatient Management of COVID-19 Patients
OVMC COVID 19 Inpatient Management Handout
- Created by Dr. Pettersen with our ID and ICU attendings
Physical & Speech Therapy Referrals
Personal Protective Equipment (PPE)
The current PPE recommendations for PUI/COVID+ patients are as follows:
ICU level care (ICU/step down) = N95 + protective eye/face shield + contact gown
Non-ICU level care
Aerosol generating procedures (AGP) = N95 + protective eye/face shield + contact gown
Non-AGP: surgical mask + protective eye/face shield + contact gown
** AGP include nebulized medications, sputum induction, HFNC, BiPAP/CPAP, intubation, bronchoscopy, or CPR
** Please contact infection control at x 73624 or x 74739 for any questions or guidance on PPEs. After hours, contact ANO x 73170
** If you have difficulty obtaining PPE, please contact the chief residents (x74411) or Dr. Suthar immediately.
Safety glasses/goggles – if you have not received a pair, please contact the Chief Residents. For UCLA/ED rotators, if your Program has provided reusable protective eye equipment, please bring it with you to your rotation. If not, please contact the Chiefs and we will provide you with a pair.]
Donning & Doffing PPE
Donning & Doffing Video from UCLA Health
DHS Guidelines for Expanded Use of N95 Respirator in Certain Clinical Circumstances
PPE Conservation
Healthcare providers should remove only gowns and gloves and perform hand hygiene between patients with the same diagnosis (COVID-19), while continuing to wear the same respiratory or face-mask and eye protection (face shield or goggles).
Obtaining Remdesivir
- Indications: Restricted to hospitalized COVID-19 patients with:
- SpO2≤94% on ambient air (at sea level) requiring supplemental oxygen via low flow device, AND
- No immediate plan for discharge…All others to require approval from Infectious Disease/COVID attending.
(Note: The NIH does not recommend starting remdesivir in those who are already intubated and/or on mechanical ventilation)
- Contraindications: Remdesivir is contraindicated or not recommended in the following situations:
- ABNL LFTs: in those with alanine transaminase or aspartate transaminase >5 times the upper limit of normal
- Renal dysfunction: Those with calculated creatinine clearance of <30 mL/minute.
Note: Pts on dialysis may be able to receive remdesivir (the drug is dialyzed) with ID Covid attending approval. - Severe disease: The NIH recommends against therapy in those with “severe” disease including pts who are intubated or on ECMO.
- Delays in therapy: Although not “contraindicated”, effectiveness of the drug is less if patients have been ill for 10 days or more.
- Permission: Although it is always appropriate to discuss a therapy with patients (or family), documentation of patient consent in the medical record is no longer required.
- Ordering: Remdesivir is now “orderable” on ORCHID (see above); please contact the pharmacy if you have any difficulties.
- Approval: Infectious disease “approval” is no longer needed provided that the ordering physician meets the above criteria.
Obtaining Convalescent Plasma
Use these instructions for obtaining convalescent plasma under the FDA Emergency Use Authorization (updated 8/26/20).
Candidates for Convalescent Plasma (interim guidance from ID division):
- confirmed diagnosis of COVID-19
- admitted to hospital
- requiring >2 L NC oxygen
- not intubated
- optimal to give within 72 hrs of diagnosis
Steps for Obtaining Plasma
- Review this document about convalescent plasma:
FACT SHEET FOR HEALTHCARE PROVIDERS
https://www.fda.gov/media/141478/download - Print this document and provide a copy to the patient or patient’s proxy
FACT SHEET FOR PATIENTS AND PARENTS/CAREGIVERS
English: https://www.fda.gov/media/141479/download Spanish: Fact-Sheet-for-Patients-and-Parents-Caregivers_spa-M9.pdf (spanish) - Obtain standard Olive View blood transfusion consent and place signed copy in paper chart
- Document a note in ORCHID confirming that you have discussed the following with the patient or proxy:
- FDA has authorized emergency use of COVID-19 convalescent plasma, which is not an FDA-approved biological product.
- The patient or caregiver has the option to accept or refuse administration of COVID-19 convalescent plasma.
- The significant known and potential risks and benefits of COVID-19 convalescent plasma and the extent to which such risks and benefits are unknown.
- Information on available alternative treatments and the risks and benefits of those alternatives.
- Order a Type & Screen
- Place Blood Product Transfusion order in ORCHID for
- Product 1 unit of plasma, specify convalescent plasma in comments
- Transfusion: specify convalescent plasma in comments
Blood Bank (x74062) will attempt to procure a unit of plasma for your patient. ID attending approval is no longer required; however feel free to page the COVID-ID attending pager (818-313-0057) with any questions.
Inpatient Rounding Policies for PUI or COVID+ Patients
Team Management during the COVID-19 pandemic
Due to the ongoing concerns for transmission of COVID 19 to healthcare workers and the need to conserve PPE, the UCLA-Olive View Internal Medicine Residency has put together this guideline for seeing PUI and COVID 19+ patients in the ED, Hospital and ICU. These are changing guidelines and are in concordance with the DHS and UCLA GME office guidelines. (Updated 7/2020)
Note: Students (medical, pharmacy, podiatry, etc.) should not examine or be assigned COVID/PUI pts.
General Expectations for Rounding and Patient Evaluations:
- All COVID-19 patients should receive the same standard of care as non-COVID patients, including timely and thorough evaluation pertinent to their disease, by house staff and attendings wearing appropriate PPE.
- If house staff or attendings feel as though they cannot appropriately care for COVID-19 patients for any reason, please discuss this with your direct supervisor and arrange for an alternative person from the team/division to take over care.
- If you are experiencing a delay in care due to PPE, or issues around the patient being COVID positive, please escalate this up your chain of command immediately, including the PD and Chair of Medicine.
- Consider bedside “discovery” rounds for all COVID-19 patients, including initial admission visit and subsequent daily rounds, with patient assessment performed during rounds.
- Consider using a WOW during rounding.
- Support each other in donning and doffing to ensure proper procedure is followed.
- Appropriate PPE consists of double gloves, gown and (CAPR/PAPR or N95 facemask + hair cover + face shield).
- Use isolation stethoscopes. When entering the room bring a chem wipe with you to clean the iso-scope prior to use.
New Admission (wards/SDU/ICU):
- After the intern gathers pertinent chart data prior to seeing the patient, the team (intern, resident and attending when possible) should see the patient together for initial assessment.
- Start the interview outside of the patient’s room together by calling into the patient’s room.
- Speak with the patient on the phone and gather all the pertinent history.
- For the initial physical exam, the attending and either the intern or resident should enter the room to examine the patient, but all members of the team need not enter the room.
- A full physical exam should be completed on all new admissions.
- The person(s) who performed the physical exam relays findings to the team.
- The team should discuss management away from the patient’s room when possible to decrease contact contamination.
- What if there is no phone in the ED?
- Ask the ED to provide a phone. After donning your PPE, place the phone inside the room, note the phone number and instruct patient on how to use the phone.
- Do an abbreviated exam pertinent to the chief complaint while in the room.
- Doff PPE and go outside to complete the expanded history and f/u with patient via phone.
- This is a backwards workflow but minimizes risk to the clinician.
Daily Rounds (wards/SDU):
- Discuss with your attending daily how rounds will run prior to evaluating the patient.
- See above for team management workflow if team rounds together.
- Decide if an in-room physical exam is needed.
- For stable COVID patients without changing O2 requirements, a daily physical exam may not be needed. Ask orientation questions every day, ability to form full sentences, and count respiratory rate from the window.
- If doing an abbreviated exam on stable patients in the room, please assess work of breathing and use of accessory muscles.
- For physical exam on stable COVID positive patients, no more than one member of the team should examine the patient in room on a given day.
- Daily progress notes should state “exam performed by Dr. X ” if the exam was done by someone other than the writer. Document the exam as you would normally – do not write a disclaimer about limited physical due to COVID. If an in-room exam was not done, please do not write “seen from window” or “not seen due to COVID”, but rather describe observed findings such as “breathing unlabored, speaking in full sentences”, etc.
- A member of the team (typically the intern) should touch base with the nurse caring for the patient daily to relay the plan for the day.
Daily rounds on non-call days (ICU):
- Speak with the patient on the phone if not intubated. If intubated, you should be able to see the vent settings from the window. Review and discuss settings with your attending on rounds.
- Decide if a physical exam in room is needed (for both intubated and non-intubated patients)
- For more stable ICU patients without changing vent requirements, this may not be necessary. Respiratory status evaluation may be done assessing the ventilator settings only, or in non-intubated patients by RR, work of breathing, etc. Discuss this with your attending.
- If a physical exam is needed, a senior member of the team should examine the patient and relay the exam findings to the rest of the team.
- Fellows and attendings should perform needed procedures in ICU COVID-19 patients, unless patient surge makes it necessary for senior residents to perform these procedures.
Consult Services:
- Consult residents should ask if the consult attending prefers the physical exam be completed by house staff BEFORE the team rounds on the patient.
- Ideally, the history should be done by the resident outside of the patient’s room via phone prior to rounding with the attending, and the attending or fellow will conduct the physical exam with the resident or intern.
- It is expected that the consult attending sees and examines all new consult patients.
- Consider bedside “discovery” rounds for all COVID-19 patients, including initial admission visit and subsequent daily rounds, with patient assessment performed during rounds.
Fellowships: See Hem-Onc Fellowship Rounding Policies on the Hem-Onc website.
Criteria for Determining Inpatient Level of Care
Please review the following criteria and please adhere to these criteria for admitting to the ICU or SDU.
ICU Admission Criteria (*requires either one major criterion or three or more minor criteria):
Major Criteria:
- Respiratory failure requiring invasive mechanical ventilation
- Respiratory insufficiency requiring high-flow nasal cannula
- Respiratory insufficiency requiring > 6 L oxygen
- Septic shock with need for vasopressors
Minor Criteria:
- Confusion
- Uremia (BUN > 20 mg/dl)
- Respiratory rate > 30 breaths/min
- Multilobar infiltrates
- Age > 55 years
- PaO2/FiO2 ≤ 300
Stepdown/Tele Admission Criteria (*requires one criteria)
- Respiratory rate >24 breaths/min
- Heart rate >125 bmp
- SpO2 <92% on room air
Bed Flow Issues – Please do not call ANO if you need a bed (including ICU). Please make sure these requests go through your attending and the day/night hospitalist to decrease confusion. If there is a bed flow issue after midnight, please page the back-up Hospitalist attending for help.
Current COVID Units:
- ICU service and level of care: 5BS 1-6; 5BN 1/2/11/12; 4BS 1-6; 4BN 1/2/11/12
- Ward service with med/surg or step-down level of care: 2F isolation unit
ICU Overflow Workflow:
When the overall ICU census is greater than 16 patients, the Department of Emergency Medicine will help with ICU overflow.
Starting 5/28/2020:
When the ICU service is full, the MICU resident will by definition be “capped” and will not be able to take on new ICU patients as the primary physician. Therefore, the DEM physicians will need to remain primary on ICU boarders (above the 16-patient cap). The ICU residents should still evaluate the patient briefly to authorize the ICU admit and give any initial recommendations, but they will not write admit orders until a bed is available.
The Pulmonary consult team will function as the ICU consult service for these boarding patients, and can assist with procedures and other management issues. The night MICU residents should sign out any ER patients over the 16 patient cap to the Pulm consult service each morning to let them know that an ICU consult is needed in the ER.
If you are finding issues with the workflow overnight, please contact the ICU fellow/attending and chief on pager. We will monitor the situation closely while maintaining upmost safety for patients and residents.
Discharge Planning: Follow-up, Home Oxygen
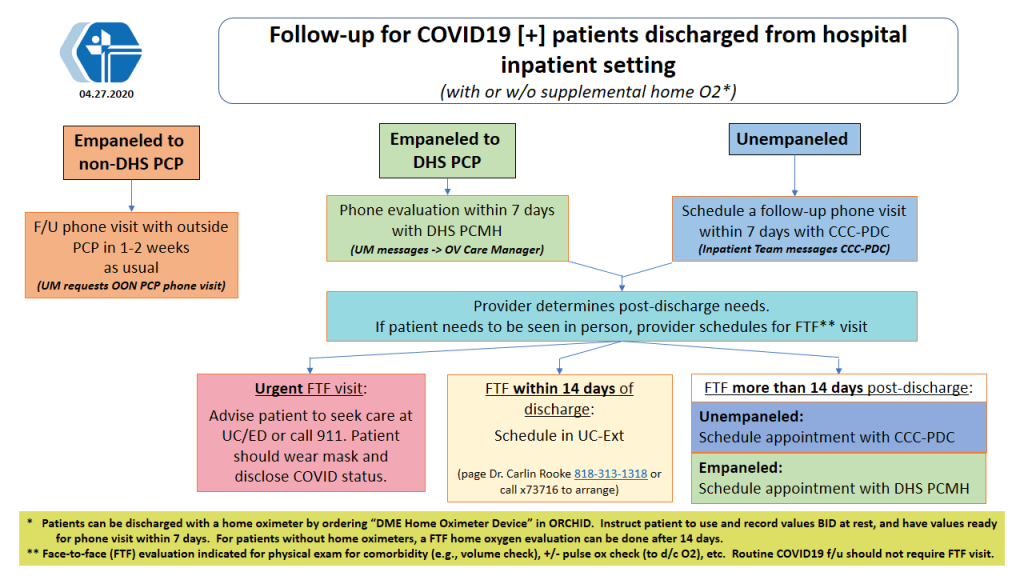
COVID-19 inpatient discharge workflow (with/without O2 needs):
Ordering Home Oxygen:
- In ORCHID, order DME home oxygen and pulse oximeter:
- DME Home Oxygen
- DME Oximeter for Home Oxygen Use
- Then, call Respiratory Therapy to alert them of the orders: RT supervisor x75038 or RT lead x75331
Helpful Patient Instructions:
Post-Discharge Follow-up
Most COVID patients being discharged with home oxygen will receive a pule oximeter and should be recommended to check twice a day at rest. Post-Discharge Clinic follow-up should be scheduled with a phone visit within 7 days of discharge.
Guidance for Evaluating COVID-19 Patients at Follow-up:
- If the patient has not checked a resting O2 sat on room air (RA), during the phone visit have the patient remove the oxygen and check the O2 sat on RA at rest.
- If the patient’s resting O2 sat on RA is less than 94%, continue home O2 and recheck with weekly phone visits.
-
- If the patient’s resting O2 sat on RA is less than 94% for at least 2 weeks after discharge, refer these patients to Pulmonary Clinic by eConsult (per Dr. Kamangar). This may be a marker of more chronic lung damage.
- When the patient’s resting O2 sat is 94% or greater, discontinue the home O2.
-
- In ORCHID, order “DME Home O2” and put “discontinue service” in the comments.
- For clinics with a Service Coordinator (for example, Kathrina Puno in Clinics A&P), message the coordinator to coordinate with the oxygen company (CalOx) to pick up the home oxygen and the oximeter.
- If no Service Coordinator, notify the RT supervisor at 747-210-5038 (M-F from 7A to 7P), who will fax the DME form to Cal Ox. For questions contact Arnold Panganiban in RT.
Notes:
- For all COVID19 patients (with or w/o home O2) who require a face-to-face (FTF) visit within 2 weeks from inpatient discharge, or 3 weeks from ED discharge, please schedule in the UC-ext by contacting Dr. Carlin Rooke or calling the Peds clinic (now UC-ext) at x73716.
- For patients on home O2 who don’t have a home oximeter and thus need a routine FTF appt to measure their O2 sat, their first oxygen evaluation can be delayed until they can see their PCP or CCC provider at least 2 weeks after hospital discharge or 3 weeks after ED discharge. If they need to be seen earlier, please schedule in the UC-ext as above.
- We’ll keep you updated about any changes in the above (and there are always changes!)
Outpatient Telehealth
We have transitioned to a mixture of Zoom and in-person precepting for outpatient resident clinics. Patients will be called by phone, and precepting will take place via Zoom, if not in-person. Please refer to the OVIM website for details including Zoom IDs and specific instructions.
Clinic A: Clinic sessions will now be a mix of telehealth visits and in-person visits for all residents. You will receive an email from Dr. Soleymani with resident/attending assignments. Please utilize this link for telephone visit guidelines:
Subspecialty Clinic Information:
- Subspecialty clinic will have a mixture of face to face visits and telephone visits
- All interns and residents will come to clinic. Attending physicians will determine which residents will see in person visits at the start of clinic. The remaining residents will do telephone visits from the hospital.
- Review tele-preceptor instructions on the website under telemedicine, if needed.
Pharmacy
For mail delivery of medications from OVMC:
- Into the eRX Note to Pharmacy, please write “mail RX today” (for new meds or refills that patient needs now) or “mail when due” (for refills needed later)
- Please include this for each medication
- Patients can follow up with pharmacy at 747-210-3066 if any issues
Housestaff Policies & Procedures
Daily Temperature Checks
Please check your temperature at home prior to coming to work or at the beginning of your shift. These temperature checks are intended to help keep everyone safe, but this depends on you to check your temperature everyday and self-report if you have a low-grade fever. Just like masking, this will only be effective if everyone does their part, so please set a reminder for yourself and remind your colleagues as well.
How to check your temperature at work:
We have infrared forehead thermometers in three locations for your convenience:
-
2nd Floor: Resident Lounge, 2C-160
-
4th Floor: 4D-104
-
5th Floor: 5B Call Suite
How to log your temperature:
The Chief Residents have posted logs in all of the ward team workrooms, ICU conference room, and the Resident Lounge. Please write your name and mark that you have checked your temperature each day.
When do I call it a fever?
If your temperature is 100°F (37.8°C) or above, please page the Chief on Call on Amion for further instructions. If you are still at home, please do not come in to work. If you are already at the hospital, please do not see patients until you have spoken with the Chief on Call.
What to Do If You Feel Sick?
If you develop symptoms (fever>100, cough, diarrhea, loss of taste/smell, shortness of breath and/or other flu-like symptoms):
- Stay at home. If onset at work, go home
- Page the Chief Resident on call immediately
- Contact OV Employee Health for drive through testing appointment (x73403) or page UCLA ID at p89294 to discuss your symptoms (you must page through mednet). They will help determine if you need COVID testing.
If you are being tested, please let the chief resident on call know.
Turnaround time for results is approx 1-2 days
Per DHS guidance, if negative for COVID, you may return to work once no fever for 24 hours, respiratory symptoms significantly improved and/or no diarrhea for 24 hours. Please contact the chief resident on call as they will help determine if you can return to work.
See PDF for further instructions:
Internal Medicine Trainee COVID-19 Flowchart “What to do if?”
Self-isolation
Hotels for Health Care Workers is a program providing hotel rooms to frontline health care workers who are exposed to or test positive for COVID-19. Please use the link for contact info. If you fall into this category, and need a place to self-isolate, please contact the Chief Residents or Dr. Suthar.
Quarantine Policies
- Stay at home. Must be off work for 14 days* from the first day of symptoms of known COVID contact. *Duration may change dependent on vaccination status
- If no mucosal exposure or respiratory secretion contact, there is no work restriction.
- Notify Chief Resident on Call or Dr. Suthar about your exposure.
- Notify your Chief Resident on Call and Dr. Suthar. Contact Infection Control first, then Employee Health.
- Follow IC/EH instructions. Asymptomatic staff will not be tested.
- Notify Dr. Suthar and Chief Resident on call immediately
- Stay home and self-isolate
- Contact Dr. Joseph Blank with employee health prior to returning to work
- Notify Chief resident on call and Dr. Suthar with return date.
See PDF for further instructions:
Internal Medicine Trainee COVID-19 Flowchart “What to do if?”
Self-isolation
Hotels for Health Care Workers is a program providing hotel rooms to frontline health care workers who are exposed to or test positive for COVID-19. Please use the link for contact info.
Food & Cafeteria
Olive Branch Cafe hours (** subject to change)
Breakfast: 7:30 AM – 10:30 AM
Lunch: 11:00 AM- 5:00 PM
Dinner: 5:00 PM – 7:00 PM
Cafe Dining Room is open 24/7 to Staff Only. The Patio is open during Cafe business hours.
Picken Park and Cogen Rooftop (next to Psych ER across the helipad) are also available to staff. Please be mindful of weather and physical distancing.
Multiple vendors & local volunteer groups have been gracious to provide boxed lunch/dinner for our residents. We will provide daily updates via pager or the WhatsApp group. The freezer in the resident lounge (2C-160, code 325) is also stocked with food for overnight/on-call residents.
** Please remember to clean up after yourselves, and ideally avoid eating at computer workstations.
Conferences/Meetings/Gatherings
Morning Reports will be occurring in- person in the auditorium to maintain physical-distancing guidelines.
Noon conferences are now taking place via zoom. The meeting ID can be found in your outlook calendar and is sent out daily during the morning page. If you do not have access to the noon conference calendar, please reach out to Dr. Ta.
Ambulatory Didactics – Some didactics will take place via zoom while some will take place in-person. See your block email for further instruction. Links to meeting IDs are on the website under ambulatory curriculum section and will be included in the weekly ambulatory block email.
What about Spring Retreat?
We are still finalizing our plans for Spring Retreat. If you have some ideas about how to best celebrate our awesome residents, please reach out to the Chiefs or PD/APDs.
Jeopardy/Surge Planning
COVID-19 Resources
Educational Resources
ICU refreshers
- ACP critical care video shorts
- OV IM website for Dr. Barot’s vent management lectures
- Curbsiders: Airway management for the non-intensivist
- SCCM: Critical Care for COVID-19 for non-ICU Clinician
Guidance on COVID-19 management
- Handout with guidance for COVID -19 Inpatient management at Olive View
-
OVMC COVID 19 Inpatient Management Handout
- Created by Dr. Pettersen with our ID and ICU attendings
-
- Handouts and Cases with guidance for COVID -19 Outpatient management at Olive View
- ATS guidance on COVID-19 management based on empiric data
- Longer read but very thorough
- ATS clinician resource page
- Includes link to COVID-19 update podcasts
- Includes link to critical care refreshers for the non crit care physician
- Curbsiders COVID-19 episode
- Interview w/ Dr. Paul Sax
- Curbsiders COVID hotcakes episode – just posted 4/10
- Goes over several of the recent COVID articles including ones about treatment with HCQ and azithromycin
- ACP Annals on Call podcast – Infection Control: Advice for physicians
- There are good diagrams accompanying the podcast
- AAFP COVID-19 Daily Research Briefs
- Get updated information on research related to COVID happening worldwide
Communicating with Patients & Families
- Check out this excellent toolkit from VitalTalk.
Public Health Information
- LA County Public Health
- Daily updates on COVID-19 cases and death toll in LA county
Wellness Resources
- Headspace
- Meditations app – healthcare workers receive free pro subscription
- DJ D-nice’s free Club Quarantine Instagram shows
- You can party with Oprah, Biden, Ellen, etc.
- @dnice
- UCLA virtual group fitness classes
- DoYogaWithMe
- 2 months of free subscription
- FYI Costco lets healthcare workers cut the line if you show your badge
- 24 hr free confidential physician support line
- Marvin
- Marvin coordinates free support sessions for healthcare professionals.
Patient Resources
- AASM Coronavirus FAQs for sleep apnea patients